Quality assurance (QA) in healthcare is often treated as a compliance exercise — something to satisfy inspectors, complete audits, and move on. That mindset is increasingly out of step with reality.
Rising patient expectations, persistent staffing pressure, and the expansion of digital and multi-channel care have made healthcare delivery more complex and more variable.
Poor quality assurance erodes patient trust, compromises outcomes, drives inefficiency through rework and complaints, and places additional strain on already stretched teams. As a result, QA can no longer sit quietly within clinical governance or audit functions.
It is a leadership responsibility, and it’s one that directly affects performance, reputation, and sustainability.
The role of quality assurance in modern healthcare
Healthcare quality assurance is here to ensure that care and service are delivered safely, effectively, consistently, and in a patient-centred way. It does that through external and internal audits, procedure reviews, staff competence assessments, performance dashboards, and other actions.
Responsibility for QA typically spans multiple roles: clinical leadership, quality or governance teams, operations, and increasingly executive management. While ownership may sit within a specific function, accountability ultimately rests with leadership.
Quality assurance is also an essential component of the overall quality management in healthcare.

Here is how quality assurance differs from (and complements) other areas of quality management:
- Quality improvement (QI) focuses on designing and implementing changes to improve outcomes. QA verifies whether standards are being met before and after those changes.
- Risk management identifies and mitigates potential harm. QA monitors whether controls and processes are actually working in practice.
- Compliance and inspection readiness ensure adherence to external requirements. QA provides the evidence base that supports compliance, rather than scrambling to assemble it.
Crucially, modern QA has shifted away from purely retrospective audits. Instead of periodic reviews looking backwards, high-performing organisations move toward continuous assurance, with a strong focus on monitoring quality in (near) real time and acting before issues escalate.
In the UK, quality assurance underpins expectations set by the NHS and the Care Quality Commission (CQC). It moves away from last-minute preparation for inspection, providing ongoing evidence of safety, effectiveness, and responsiveness.
This makes organisations ready for inspections: their data, processes, and improvement actions already exist and — if the system is digitised — can be easily transformed into a report on request.
Why healthcare quality assurance matters more than ever
Several structural pressures have raised the stakes for QA.
Workforce shortages and burnout increase variation in care delivery, especially in patient-facing interactions. New staff, rotating teams, and reliance on temporary capacity make maintaining consistency difficult without strong quality oversight.
At the same time, care is no longer confined to a single setting. Digital consultations, remote triage, asynchronous communication, and outsourced services all expand the number of touchpoints where quality can degrade — and this often happens outside traditional clinical review processes.
Scrutiny has also intensified: regulators, commissioners, patients, and the public have greater access to information and higher expectations of transparency. When quality fails, it is visible quickly and at scale.
There is, naturally, a direct financial impact as well. Poor quality drives complaints, rework, litigation, staff turnover, and reputational damage, all of which carry real costs. From an executive perspective, QA is a lever for operational efficiency and performance improvement.
The building blocks of an effective healthcare QA program
Strong QA programs share a small number of foundational elements. Let’s dive deeper into those.
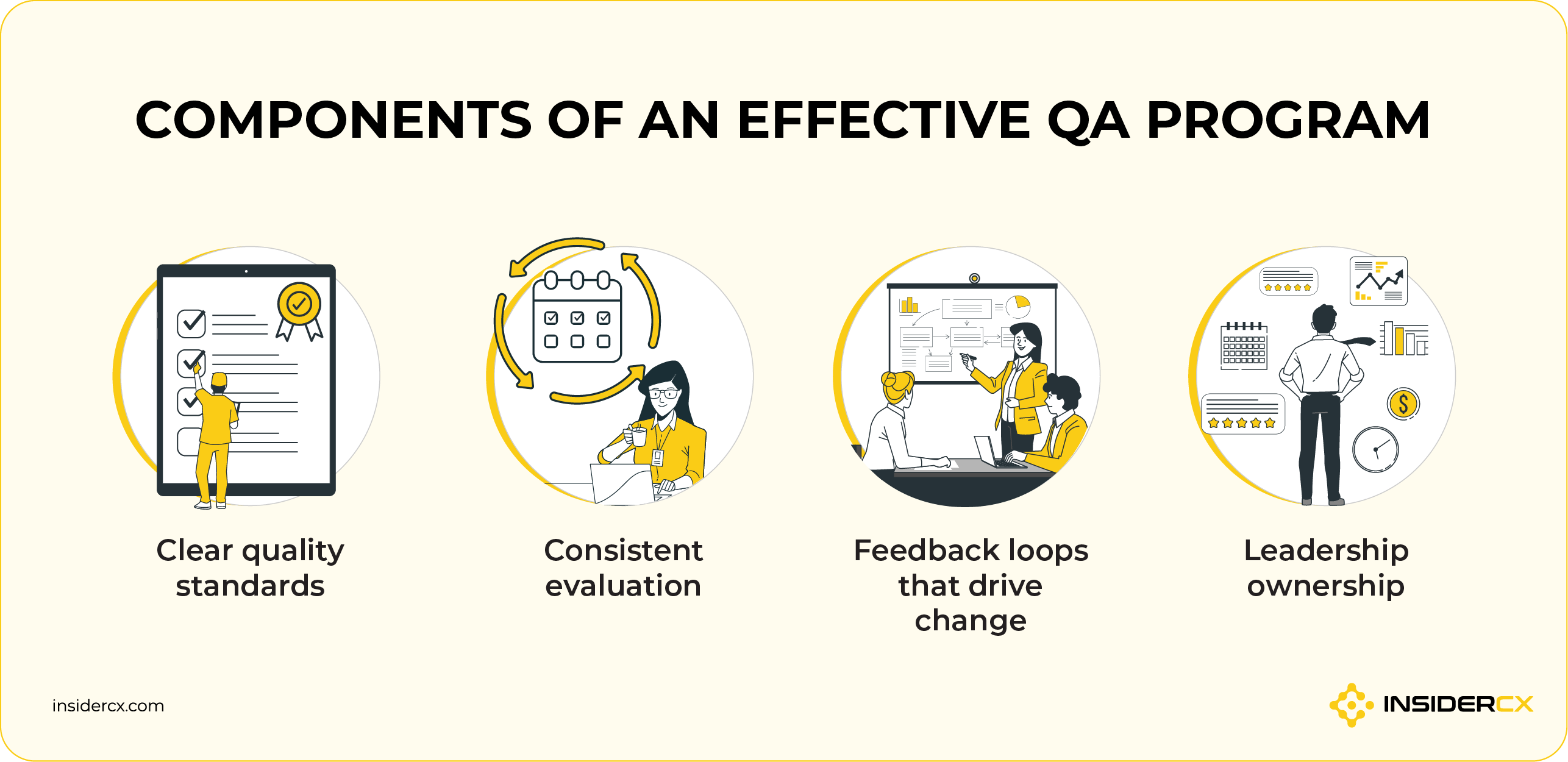
1. Clear quality standards
Quality assurance begins with clarity. Organisations must define what “good” looks like across key dimensions, including:
- Clinical safety and adherence to protocols.
- Communication, compassion, and respect.
- Timeliness, access, and continuity of care.
These standards must be observable and measurable. Vague aspirations are difficult to assess and impossible to enforce consistently; clear criteria enable fair evaluation and constructive feedback.
A quick example:
- Vague and aspirational: “Patients should feel well informed and supported.”
- Observable and standardized: “Before discharge, clinicians confirm that the patient received written aftercare instructions, understands next steps, and knows who to contact with questions.”
The first objective expresses intent, but offers nothing to evaluate consistently. The second defines a behaviour that can be observed, measured, and reviewed — which is exactly what quality assurance requires.
2. Consistent evaluation
Sporadic audits create blind spots. Effective QA relies on structured, repeatable evaluation that happens regularly and across a representative sample of activity.
This means balancing quantitative scoring with qualitative insight, and extending QA beyond clinical documentation to include patient-facing interactions — consultations, calls, messages, and follow-up communication.
3. Feedback loops that drive change
QA only delivers value when findings lead to action. Effective programs ensure that insights:
- Inform coaching, supervision, and training.
- Influence process and care pathway redesign.
- Appear in leadership dashboards alongside other performance metrics.
Closing the loop visibly is critical. When staff see that feedback leads to support and improvement — not blame — trust in the QA process grows.
Here’s an example: A clinic identifies that patient dissatisfaction clusters around unclear discharge instructions. Instead of retraining individuals in isolation, leadership revises standard discharge templates, reinforces communication expectations, and tracks improvement through follow-up audits and patient feedback.
4. Leadership ownership
Quality assurance requires executive sponsorship. When leaders engage with QA metrics, and discuss them alongside financial and operational KPIs, it sends a clear signal that quality is central to performance.
Keep in mind that QA works best as a tool for improvement rather than surveillance. Plus, it ensures that systemic issues identified through QA receive the attention and resources they require.
Best QA practices from high-performing clinics
High-performing clinics treat quality assurance as part of everyday operations, not a special project. Here’s how:
- They embed QA into routine workflows rather than running isolated initiatives.
- They focus on trends and root causes instead of reacting to one-off failures.
- They use QA to support staff development, not to police behaviour.
- They align QA priorities with patient experience, access, and service design.
- They regularly revisit and refine quality criteria as services evolve.
Example: A provider facing rising complaints initially considers adding capacity. QA analysis reveals that complaints stem primarily from unclear communication, not access. Improving consultation structure and follow-up messaging reduces complaints without increasing staffing levels.
How technology strengthens quality assurance in healthcare
Manual QA processes are almost impossible to scale in modern healthcare. Limited samples, inconsistent reviews, and delayed reporting reduce their effectiveness while complexity increases.
Technology does not replace professional judgement. It significantly strengthens QA by:
- Expanding coverage so more interactions can be reviewed.
- Improving consistency and objectivity through structured scoring.
- Surfacing patterns and risks that would otherwise remain hidden.
Technology-enabled QA may include monitoring patient interactions, automated quality scoring against defined standards, and trend analysis across services, teams, or locations. Used well, these tools help leaders move from reactive oversight to proactive assurance.
The result is not automation for its own sake, but better visibility, earlier intervention, and more confident leadership decisions, which is exactly what quality assurance is meant to support.
Practical first steps for healthcare leaders
Strengthening quality assurance doesn’t require a wholesale transformation on day one. The most effective leaders start by creating clarity, narrowing focus, and building momentum through small, deliberate steps that compound over time. Below is a rough step-by-step guide.
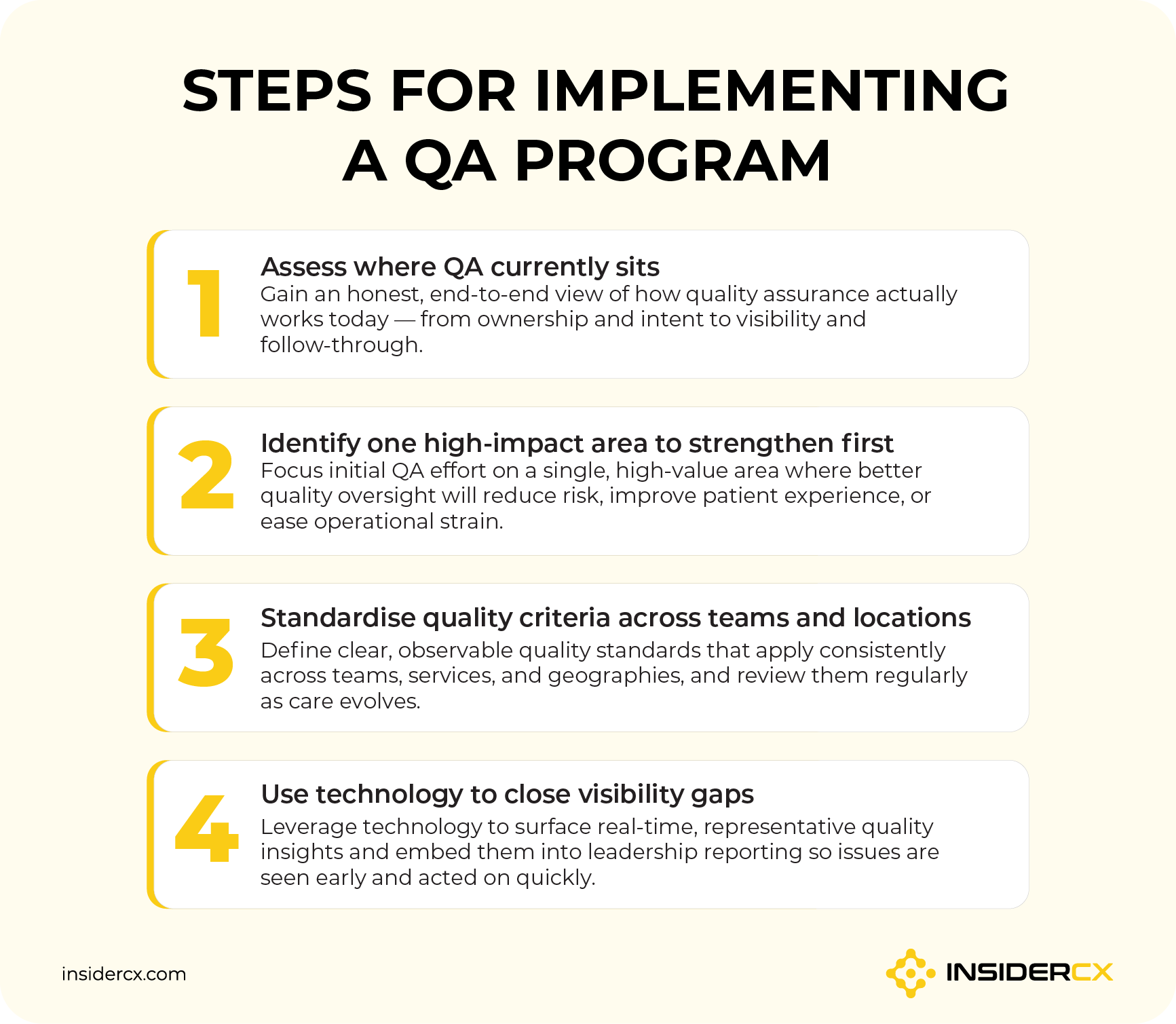
1. Assess where QA currently sits
Before changing anything, leaders need a clear picture of how quality assurance functions today. This assessment should be honest and practical, not theoretical.
- Clarify the primary purpose of current QA efforts — whether they exist mainly for compliance, continuous improvement, operational insight, or a mix of all three.
- Identify who owns QA today and how responsibilities are distributed across clinical leadership, operations, governance, and frontline teams.
- Evaluate how QA findings are captured and reported, including what happens to insights once they are identified and who is responsible for acting on them.
- Assess leadership visibility, comparing what executives regularly see in reports with what frontline teams experience in daily care delivery.
- Identify gaps between intent and execution, i.e. where the stated QA goals are not consistently reflected in day-to-day practice.
2. Identify one high-impact area to strengthen first
Attempting to fix everything at once usually leads to diluted effort and limited impact. In most cases, leaders should select a single area where improved QA can deliver clear value.
Priority areas often share common characteristics. They:
- Affect a large proportion of patients.
- Generate frequent complaints or pose elevated risk.
- Create operational inefficiency, rework, or avoidable staff frustration.
Common starting points include patient access, discharge processes, or communication quality across key touchpoints.
Once a focus area is chosen, it’s essential to define what success looks like — both in qualitative terms and through simple, trackable measures — so progress can be clearly demonstrated.
3. Standardise quality criteria across teams and locations
Inconsistent standards undermine QA efforts. Leaders should ensure that “good quality” is defined in terms that teams can observe, measure, and apply consistently.
This includes aligning quality criteria across clinical, operational, and patient experience teams so everyone works toward the same expectations. It should also apply regardless of whether a patient is seen in London, Zagreb, or Madrid. Just as importantly, there should be a structured review process to revisit and update standards as services, pathways, and patient needs evolve.
Optical Express, a leading eye care provider with almost 130 clinics across five countries, faced just this challenge — significant variation in patient intake flows and quality measurement across borders and service lines.
Using a structured, automated feedback loop via the InsiderCX platform, they were able to benchmark satisfaction and identify quality gaps across all clinics and external partners. The result was a 23% month-on-month increase in Net Promoter Score (NPS).
4. Use technology to close visibility gaps
Technology plays a critical role in helping leaders see what is actually happening across their organisation. Well-designed systems can surface trends, highlight risk indicators, and reveal variation in performance that manual processes often miss.
Below are some of the key technology categories that strengthen QA and how they each contribute:
- Patient feedback and experience platforms: Consistently capture structured feedback across the patient journey and turn it into quantifiable insights that show where quality is strong or weak in real time. 
- Quality monitoring tools: Automatically review interactions (such as calls or messages) against predefined criteria so teams don’t have to manually sample to identify quality gaps.
- Analytics and reporting platforms: Aggregate data from QA activities and other sources into dashboards that highlight trends, outliers, and performance variation across teams or locations. 
- Automated audit and scoring systems: Convert quality criteria into standardised scores so evaluations are objective and comparable across services and over time.
QA insights should feed directly into existing leadership reporting, rather than living in isolated dashboards. Used this way, technology supports better human decision-making: it doesn’t replace professional judgement, but it ensures leaders are acting on timely, representative information.
Quality assurance as a strategic advantage
Quality assurance is not about avoiding failure at all costs. It is about creating the conditions for consistency, trust, and resilience in complex healthcare environments.
Organisations that invest in QA are able to deliver reliable outcomes, support their workforce through clarity and feedback, and adapt as expectations, technologies, and pressures evolve.
For healthcare leaders, QA remains one of the most controllable — and yet, underutilised — levers for sustainable improvement.
Want to find out your clinic’s current quaality management maturity? Begin with the keystone — your feedback system — by completing InsiderCX’s free feedback management system assessment.




