Quality management (QM) systems are often designed so that they tick regulatory boxes. But they should be much more than that.
A 2023 multi-country analysis found that hospitals in the top quartile for patient-reported experience achieved both higher total revenue and lower per-case costs. On the compliance front, accreditation bodies such as the Joint Commission in the U.S. explicitly link their standards to continuous-improvement methods.
To put it bluntly, clinics that invest in structured QM consistently report higher patient-experience scores and generate greater revenue while lowering complication-related costs.
Let’s define quality management in healthcare, highlight the benefits clinics gain when they practice it effectively, and break down the four core components every QM programme must include.
What is quality management in healthcare?
Quality management in healthcare encompasses a range of coordinated systems, policies, and processes that minimise harm, optimise outcomes, and ensure services consistently fulfil their intended purpose.
With its ultimate goal being to make each patient encounter both safe and effective, here are the major benefits of effective QM:
- Higher patient satisfaction and loyalty: Experience scores improve when processes are standardised and staff are empowered to solve problems.
- Better financial performance: Private clinics with strong patient experience attract more patients and generate higher revenue.
- Regulatory and medico-legal protection: Demonstrating proactive QM helps meet state or national quality mandates and can reduce malpractice exposure.
- Operational efficiency and cost control: Eliminating rework, errors, and waste from internal processes frees capacity and trims overhead.
- Enhanced reputation and market share: ISO-certified health organisations, for example, gain global recognition and patient trust.
Robust QM practices are also the mechanism clinics use to comply with — and prove compliance to — national and international benchmarks (such as ISO 9001:2015).
Integrating these external standards into everyday practice ensures that regulatory compliance and quality improvement progress together, rather than in parallel tracks.
The four core components of healthcare quality management
Every successful healthcare quality management system, whether built for a private dental clinic or a tertiary hospital, rests on four interlocking pillars. In the following sections, we will examine each pillar and demonstrate how they mutually reinforce one another.

1) Quality planning
Quality planning is the foundation of any effective quality management system. In healthcare, it’s the process of identifying what “high-quality care” means for your clinic — and then putting a plan in place to achieve it.
At its core, quality planning involves setting clear quality goals (like improving patient wait times or reducing medication errors) that align with patient needs, clinical best practices, regulatory requirements, and the clinic’s broader business strategy.
Once these objectives are defined, the next step is to design the systems and processes that will support them. This includes developing policies, procedures, and workflows that guide staff in delivering care consistently and safely.
For example, planning may involve establishing protocols for collecting and verifying patient information, scheduling follow-up care, and handling and escalating complaints.
Here are some tools and methods commonly used in quality planning:
- SWOT analysis: To evaluate internal strengths and weaknesses, as well as external opportunities and threats related to quality.
- SMART goals: Ensuring that quality objectives you set are Specific, Measurable, Achievable, Relevant, and Time-bound.
- Patient Journey Mapping: Visualizing the steps a patient takes through your clinic to identify where quality can be improved.
- Risk Assessment Tools: Methods like FMEA (Failure Modes and Effects Analysis), Root Cause Analysis (RCA), and Fault Tree Analysis (FTA) help anticipate where processes might break down and proactively plan to prevent errors.
- Benchmarking: Comparing your clinic’s performance against peers or industry standards.
- Stakeholder input sessions: Involving staff and patients in identifying quality priorities and practical barriers.
Effective quality planning is proactive, not reactive. It helps set the direction for your clinic’s quality efforts and ensures that improvements are intentional, measurable, and sustainable.
2) Quality control
While quality planning sets the vision, quality control (QC) is all about making sure that day-to-day operations are actually delivering on that vision. It involves monitoring clinical and administrative activities to identify errors, ensure consistency, and verify that services meet the established quality standards.
In a private clinic setting, quality control can include everything from checking that patient records are complete and accurate to ensuring that sterilization protocols are being followed correctly, or verifying that the average patient wait time is within acceptable limits.
QC isn't just about finding faults — it’s about creating systems that prevent mistakes from happening in the first place, and quickly catching them when they do. The goal is to maintain a stable, predictable level of quality across all services.
When it comes to quality control, here are the go-to methods:
- Checklists and protocols: Standardized procedures help staff follow best practices consistently — for example, a daily checklist for equipment sterilization or medication reconciliation.
- Audits and spot checks: Internal or external reviews of processes (e.g., chart audits, hygiene audits) to confirm that policies are being followed.
- Process control charts: Visual tools used to track variations in performance (e.g., patient wait times or lab turnaround times) and identify trends outside acceptable limits.
- Error and incident tracking systems: Tools for logging, categorizing, and analyzing incidents, near misses, or non-conformities — often integrated into quality software or patient experience platforms.
- Compliance monitoring: Regular reviews to ensure adherence to local regulations, accreditation standards, or internal benchmarks.
Quality control is a frontline defense — it helps prevent small mistakes from turning into bigger problems that impact patient safety, satisfaction, or outcomes. It also gives clinic leaders and quality managers the real-time insight needed to course-correct when things start slipping.
3) Quality assurance
If quality control is about catching issues in real-time, quality assurance (QA) is about building confidence that your clinic’s systems are working as intended. It’s a more system-wide, proactive approach that ensures processes are not only being followed but are also effective in delivering high-quality care over time.
QA involves reviewing operations, evaluating adherence to protocols, and making sure that clinical and administrative processes are both compliant and optimized. The goal is to guarantee quality — not leave it to chance.
Quality assurance also plays a crucial role in ensuring regulatory compliance, readiness for accreditation, and mitigating risk. It helps uncover whether your policies are being applied consistently across the clinic and whether your outcomes align with your intended standards.
Tools and methods commonly used in Quality Assurance:
- Internal audits: Systematic reviews of clinical, operational, and administrative processes to evaluate whether policies and procedures are being followed.
- Policy and procedure reviews: Routine assessments to ensure protocols are current, aligned with best practices, and properly communicated to staff.
- Performance dashboards: Aggregated KPIs across departments to track quality metrics over time and flag areas needing attention.
- Accreditation readiness checks: Structured walkthroughs or mock inspections to prepare for external reviews (e.g., ISO, Joint Commission, local health authorities).
- Staff competency assessments: Verifying that team members are trained, credentialed, and up-to-date on required skills and practices.
- Standard Operating Procedure (SOP) compliance monitoring: Ensuring that SOPs are being consistently applied in real-world scenarios.
Unlike QC, which tends to be task-focused and reactive, QA takes a broader, more preventive view. It focuses on whether your systems are strong enough to consistently deliver the level of care you’ve planned for.
4) Quality improvement
Quality improvement (QI) is the continuous, data-driven effort to close performance gaps and fix inefficiencies revealed by QC and QA.
In a private clinic, QI might involve reducing patient wait times, improving appointment scheduling, increasing patient follow-up compliance, or enhancing communication between departments. It’s often focused on factors that impact the overall patient experience.
What can clinics actually do for their QI efforts?
- PDSA cycles: A simple but powerful method for testing and implementing changes on a small scale before full rollout. You can run rapid 30 to 90-day experiments (test a change, study results, and scale what works).
- Lean methodology: Focuses on eliminating waste in processes (e.g., redundant forms or unnecessary hand-offs) to improve efficiency and value to patients.
- Six sigma (DMAIC): A data-driven approach aimed at reducing variation and minimizing errors in clinical and operational processes.
- Patient and staff feedback: Surveys, suggestion boxes, or interviews used to identify improvement opportunities directly from those experiencing or delivering care.
- Balanced scorecards: A structured way to track performance across multiple domains — not just clinical outcomes, but also financial, operational, and patient satisfaction metrics.
Quality improvement is how a good clinic becomes a great one — by creating a culture where feedback is welcomed, data drives decisions, and experimentation is encouraged in the pursuit of better outcomes.
How different roles contribute to quality management processes
Quality management is a team effort. Of course, some roles are more hands-on with quality systems and metrics, while others support the bigger picture through day-to-day actions. Here’s how the key players contribute:
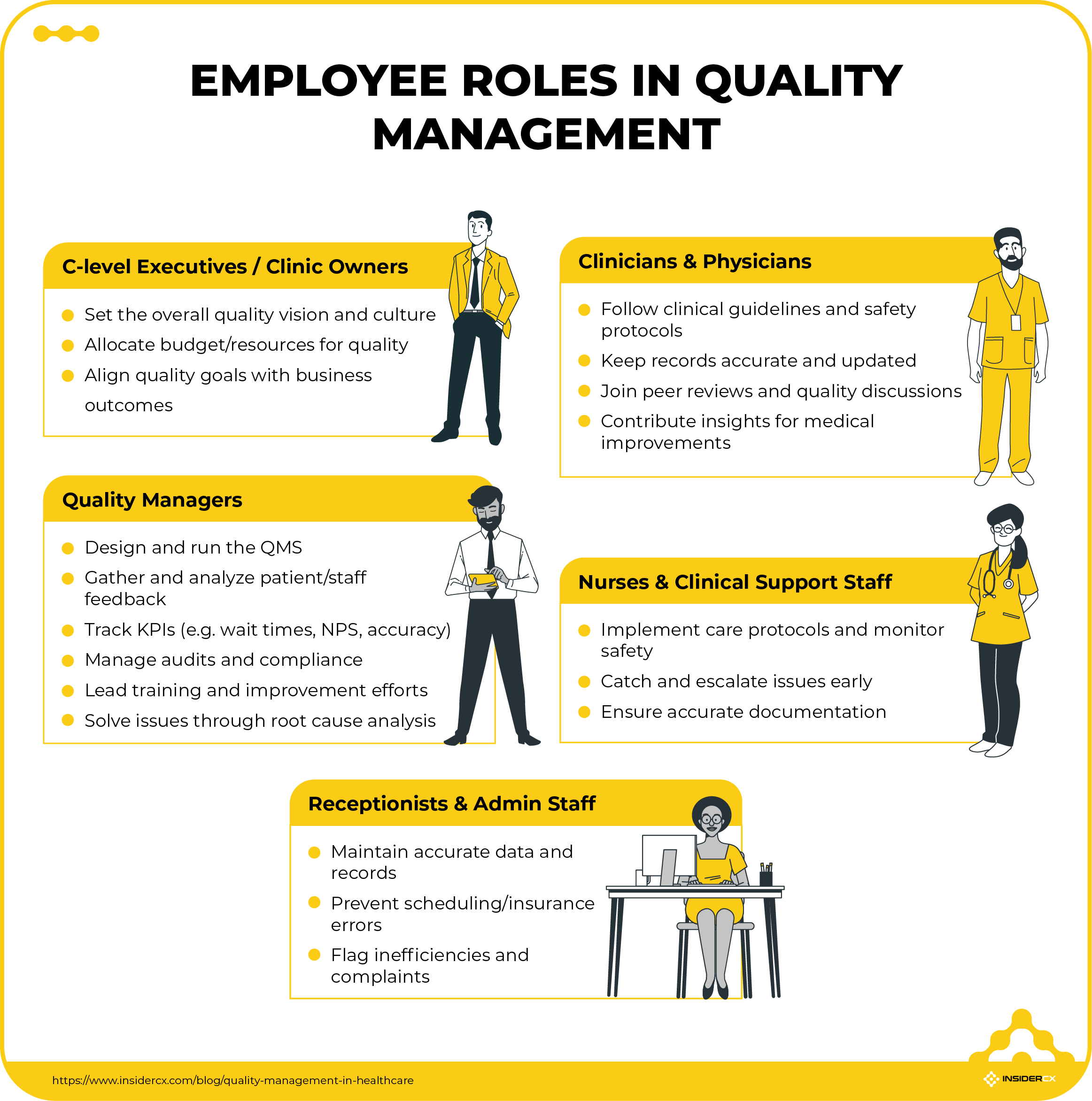
1) C-level executives / Clinic owners
As the strategic leaders, executives and owners set the tone for quality across the organization:
- They define the overall vision for quality and ensure it's baked into the clinic’s culture.
- They allocate the budget and resources needed for quality initiatives, training, and tools.
- They keep quality goals aligned with business outcomes — like patient retention, reputation, and clinic revenue.
2) Quality managers
Quality managers are the engines behind the clinic’s quality management system — both its design and day-to-day operation. They:
- Lead the development of quality frameworks, policies, and procedures.
- Set up systems for gathering and analyzing patient and staff feedback — including surveys, complaints, and incident reporting.
- Track and report on KPIs like patient wait times, NPS score, satisfaction rates, or documentation accuracy.
- Coordinate audits, regulatory compliance, and continuous improvement efforts.
- Facilitate staff training, cross-functional collaboration, and culture-building initiatives focused on quality.
- Dig into root causes and drive solutions when something goes wrong.
3) Clinicians & physicians
Clinicians are at the heart of care delivery, and their commitment to quality directly affects patient outcomes:
- They follow evidence-based clinical guidelines, protocols, and patient safety standards.
- Keep patient records accurate and up to date — which supports both care coordination and compliance.
- Participate in peer reviews, safety reporting, and improvement discussions.
- Their insights often drive medical quality improvement efforts.
4) Nurses & clinical support staff
Nurses and support staff are on the frontlines, turning protocols into real-world care:
- They follow safety procedures, monitor patients, and ensure that clinical workflows are followed precisely.
- They’re often the first to catch issues — like patient distress or a missed handoff.
- Accurate documentation and timely escalation of problems make them vital to quality assurance.
5) Receptionists & administrative staff
While not involved in clinical care, admin staff are key to a smooth, high-quality patient experience:
- They are responsible for maintaining data accuracy in scheduling, patient intake, and record-keeping systems.
- A well-trained front desk team can prevent errors before they happen — like mix-ups in appointments or insurance issues.
- Provide valuable insights into administrative inefficiencies and patient complaints.
Want to deliver safer, smoother, and more person-centered care? Then every employee needs to play their part in the quality management process.
Common challenges in implementing quality improvements
Even the most carefully crafted quality-management plan will encounter roadblocks once it meets day-to-day reality. Understanding these common obstacles — and planning concrete ways to overcome them — is the thing that makes the difference between initiatives that stall and those that translate into lasting improvements.

1) Resistance to change among staff
Even well-designed quality programmes can stall when frontline staff feel excluded or overloaded. The result is slow adoption of new protocols, inconsistent use of checklists, and a persistent “that’s not how we do things here” attitude.
Potential fixes:
- Co-create the change: Invite nurses, physicians, and clerical staff to shape the new process so it feels like their idea.
- Frame the “why” in patient terms: Show how the change reduces harm or hassle for real people, not just metrics.
- Start with quick wins: Pilot on a single shift or unit to demonstrate success before scaling.
- Pair champions with sceptics: Peer-to-peer coaching often beats top-down mandates.
2) Poor communication between departments
Silos are a perennial enemy of seamless care: lab results arrive late, imaging studies go unreviewed, and patients bounce between units repeating the same story. Miscommunication inflates length. You end up with frustrated patients and frustrated staff.
A robust hand-off protocol — whether an electronic dashboard that flags pending tasks or a simple SBAR (Situation-Background-Assessment-Recommendation) script — turns departmental borders into smooth relay zones. Regular cross-department huddles further iron out misunderstandings before they reach the patient.
3) Lack of time or resources for quality initiatives
Clinicians already juggle heavy caseloads. Add documentation demands, and the bandwidth for improvement work shrinks rapidly. When staff view QI as “extra” work, projects languish and enthusiasm fades.
Embedding improvement tasks into normal workflows solves much of the strain.
For instance, a five-minute end-of-shift debrief can capture ideas for the next PDSA cycle. Allocating protected time — one afternoon per month — for each unit to review its metrics and plan adjustments signals leadership commitment and prevents quality from becoming an after-hours hobby.
4) Inadequate data collection or analysis
Without timely and trustworthy data, teams fly blind; they can’t see whether the changes they implement help or hinder. Quality managers end up making decisions based on anecdotes that do not accurately reflect the actual situation on the clinic floor.
Potential fixes:
- Automate data capture directly from the EHR to cut manual tallying and transcription errors.
- Build patient surveys the right way to get unbiased answers and automate patient feedback collection using digital forms to minimize human error.
- Standardise definitions (e.g., what counts as “left without being seen”) so every report measures the same thing.
- Visualise in real time with simple run or control charts at unit level — instant feedback beats month-end spreadsheets.
- Upskill staff in basic data-literacy workshops so frontline teams own, trust, and act on their numbers.
5) Balancing cost control with quality efforts
Finance teams may view quality improvement as an expense centre, while clinicians fear that aggressive cost-cutting will erode care standards. The tension can freeze decision-making: initiatives stall as leaders debate ROI versus patient benefit.
But it doesn’t have to be a trade-off. The key is to reframe quality and cost as partners, not competitors. For example, streamlining your patient intake process using digital forms can reduce admin workload and improve the patient experience by cutting down on wait times and errors.
Another smart move is to bundle improvement ideas with a clear business case. If you can show how a proposal will save money, reduce risk, or even grow revenue — while also improving outcomes — you're far more likely to get executive buy-in.
Using software to simplify healthcare quality management
High-performing private clinics treat quality management as a growth engine, not a compliance chore. Why? Because stronger patient experience drives loyalty and revenue, and the payoff justifies proactive investment in the systems, training, and culture.
Modern patient-experience platforms — such as InsiderCX — streamline the cycle by automatically capturing multi-channel feedback, surfacing real-time alerts on emerging issues, and linking staff actions to quality metrics.
Clinics using digital feedback engines report faster problem resolution and measurable gains in both experience scores and clinical outcomes.
Take five minutes to gauge your clinic’s current QM maturity. Begin with the keystone — your feedback system — by completing InsiderCX’s free feedback management system assessment.




