Improving care quality has become much more than an ethical aspiration. These days, it is a direct driver of a clinic’s reputation, revenue, and regulatory standing. Studies show that hospitals and clinics earning higher patient-experience scores attract more patients and generate greater revenue while containing costs.
On the other end of the spectrum, poor care quality or safety lapses can trigger fines, licence restrictions, or even forced closure under modern compliance regimes. In short — quality is now a board-level metric as well as a bedside concern.
This article clarifies what “high-quality care” means, offers six practical improvements you can begin this month, and closes with the key metrics you’ll need to prove progress.
What does it mean to deliver high-quality patient care?
Quality of care describes how effectively healthcare services for individuals and communities raise the chances of achieving the desired health outcomes. Healthcare quality is commonly defined by six domains first articulated by the U.S. Institute of Medicine:
- Safe and effective: Care is evidence-based, avoids unnecessary variation, and reliably achieves the desired clinical outcomes — while avoiding preventable harm.
- Patient-centred: Services respect each patient’s preferences, needs, and values, with those values guiding decisions.
- Timely: Delays that could cause harm or frustration (e.g., long waits, slow test results) are minimised.
- Equitable: Quality does not vary due to factors such as gender, ethnicity, income, or geography.
- Efficient: Resources (people, rooms, equipment) are organised so that maximum value reaches the patient with minimal waste.
Strategies for improving patient care
Delivering better care does not require a multimillion-dollar rebuild or a two-year transformation plan. Below you’ll find six proven levers you can start pulling this month, along with the evidence showing why each pays off.
Move quickly, track what happens, and then iterate!
1) Actively use patient feedback to guide improvements
Patients rarely complain about medical science, but they do complain about how it is delivered. That makes structured feedback your single richest source of care quality improvement ideas.
Your goal is to systematically send post-visit surveys — and then analyse them. You’re likely to see significant gains in overall satisfaction before any clinical metrics shift.
To do that efficiently, put feedback on an assembly line:
- Collect patient feedback automatically — via SMS with links, QR posters, or online review scraping.
- Distil recurring pain points — “wait time”, “rushed explanations”, “billing clarity”.
- Act & advertise — publish “You spoke, we listened” boards in the reception area and echo them in email updates.
2) Invest in staff training and engagement
A great website cannot offset a single curt remark at the desk. Regular micro-training in empathic communication, cultural competence, and “service recovery” techniques cuts complaints and raises scores.
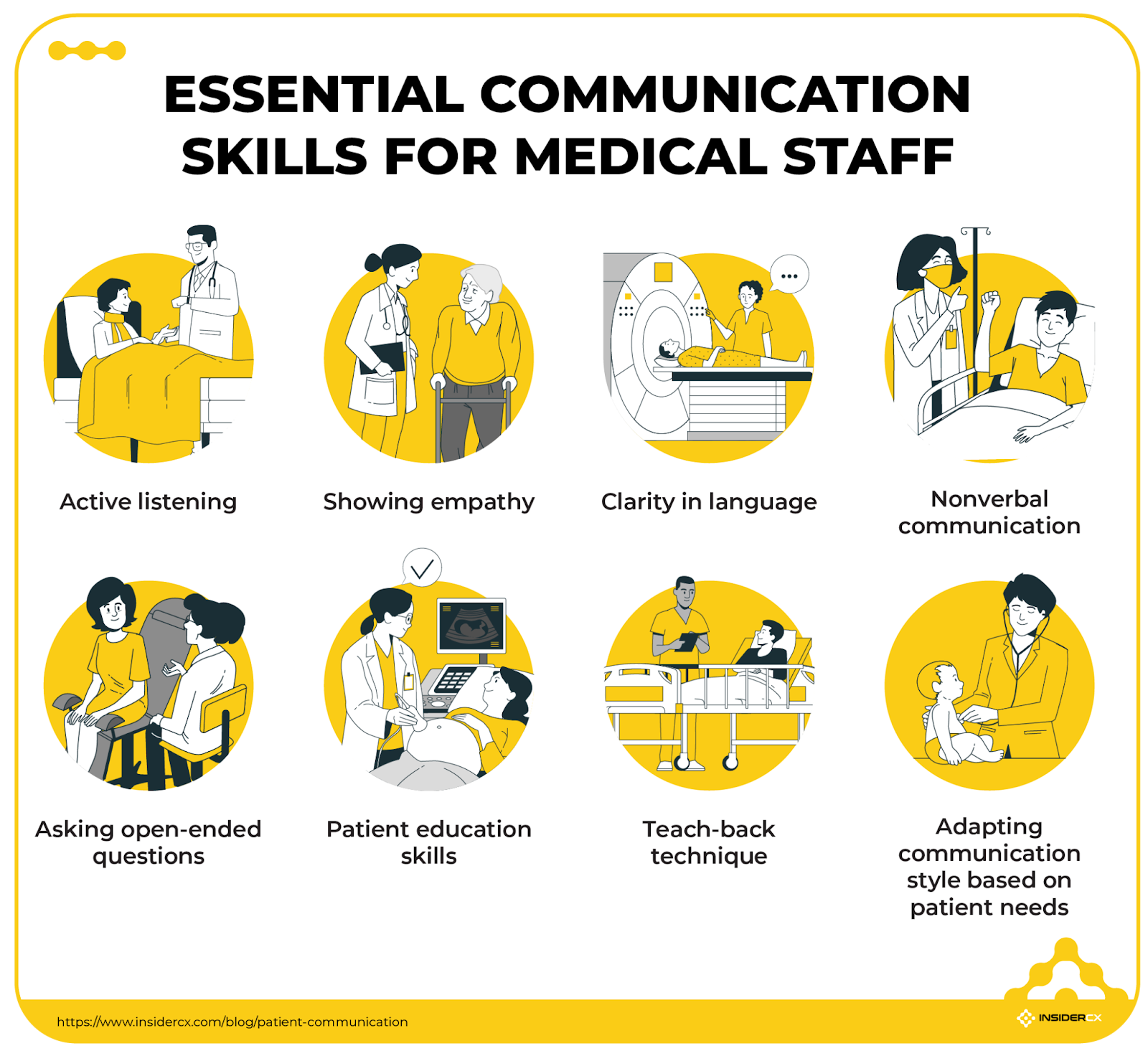
But competence without commitment is half a strategy. Recognise behaviour that protects safety or delights a patient — on-the-spot thank-you cards, a monthly “quality champion” pin, a small gift card — and watch discretionary effort surge.
3) Standardize clinical and service protocols
From surgery to spirometry, variation is the enemy of safety. The WHO Surgical Safety Checklist alone has been linked to a drop in complications across multiple meta-analyses. Private clinics can adopt the same philosophy:
- A triage checklist ensures urgent cases bypass routine queues.
- Front-desk scripts guarantee every caller hears the same clear explanation of preparation instructions or how to reschedule an appointment.
- Monthly audits (five random charts per clinician) reveal drift before it becomes a risk.
In the long run, if everyone follows the same reliable path, the clinic is bound to see a steady increase in satisfaction, positive reviews, and patient retention.
4) Empower and engage patients in their care
Active patients take their medicines, keep their follow-ups, and spot early warning signs themselves. Higher engagement scores usually lead to better glycaemic control, meeting blood-pressure targets, and improved post-operative recovery — in other words, better care outcomes.
Make it easy by:
- Translating each diagnosis into plain language (“You have Type 2 diabetes; here’s what that means day-to-day”).
- Using shared-decision charts so the patient picks the treatment path that best fits work, family, or cultural realities.
- Backing it up with a portal, printed leaflets, and a post-visit SMS recap. Adherence reviews like these tie better outcomes directly to your clinic’s experience scores.
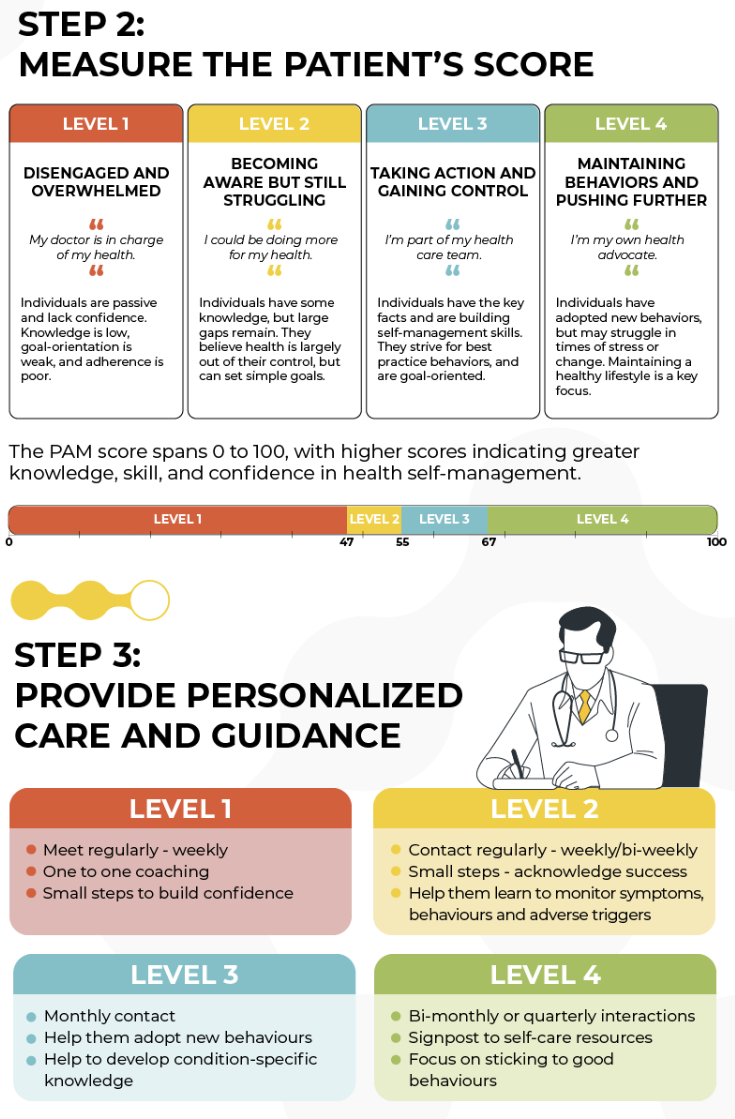
For chronic patients (or those with a long recovery process), the most effective approach is to measure patient activation level directly through PAM surveys — then adjusting your approach and communication accordingly.
5) Leverage technology to improve access and flow
Every minute a clinician spends chasing forms is a minute lost to dialogue. Digital self-scheduling shortens appointment lead time and cuts no-shows: one 2024 outpatient study found online-booked slots missed only 1.8% of the time versus 5.9% for phone bookings.
Automated reminders (SMS, WhatsApp) can further reduce missed appointments, while e-forms that push history straight into your EHR system mean the first minutes of each consultation are about people, not paperwork.
6) Start small but act decisively
NHS offers a great guide on how to use Plan-Do-Study-Act (PDSA) cycles to improve patient care . The method’s power lies in its speed: plan a small change, test it over days or weeks, study the data, and act on what you find.
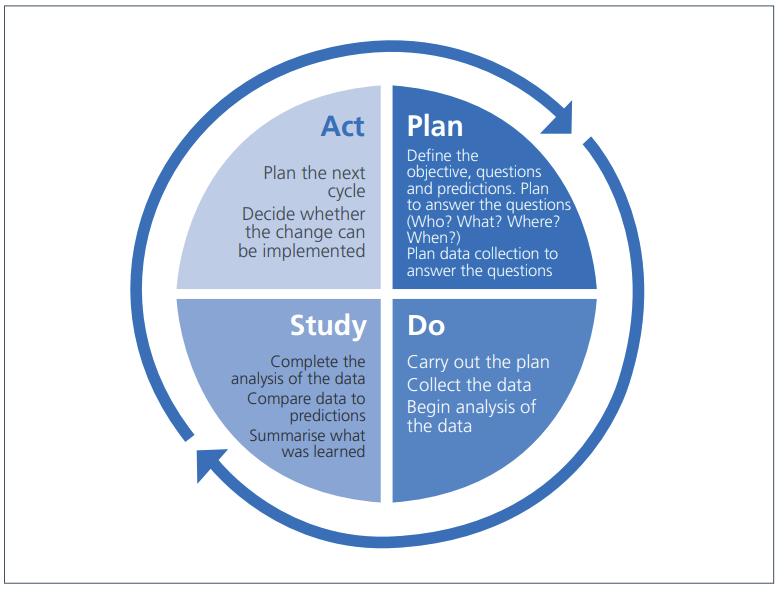
Example:
- Problem — average waiting-room time is 25 minutes.
- Plan — start clinics ten minutes earlier and add a floating medical assistant.
- Do — pilot on Tuesdays for four weeks.
- Study — daily run-chart shows wait-time median falls to 14 minutes by week three.
- Act — roll out the change to all days; launch the next cycle, focused on discharge instructions.
Quick wins galvanise staff and prove to owners that quality drives efficiency, not expense.
Bottom line: choose one lever, pull it hard for a month, measure, share the story — then move to the next. Continuous momentum beats “big-bang” makeovers every time!
Measuring care quality improvements
Better outcomes and fewer complications remain the gold standard, but day-to-day management needs more granular, leading indicators — collect these monthly, review trends quarterly, and link changes back to the specific interventions you introduced.
Here’s where to start:
- Net Promoter Score (NPS): A strong proxy for loyalty; healthcare NPS above +50 is considered excellent.
- Online review ratings: Google Reviews, Trustpilot, and similar review sites can heavily influence patient choice. More importantly, you can use them to gather feedback and track complaints, identifying areas that need improvement.
- Repeat-visit and retention rate: Indicates trust and continuity of care.
- Time to appointment: Directly affects timeliness and revenue.
- Patient throughput per provider session: Balances efficiency with quality.
- Staff satisfaction/turnover: Low engagement predicts a number of possible incidents, including safety events.
You can also go deeper with InsiderCX topic-level sentiment analysis. For example, one client consistently received a 43.8% negative sentiment score for facilities — and this rating rarely exceeded 27% for their other locations. In another case, we identified a 60.1% negative score related to appointment punctuality and duration, while staff-related feedback scored far better.
These insights help pinpoint exactly where service delivery is faltering — and where it’s working. They implemented changes to improve patient experience, which, in most cases, is the same thing as improving care quality.
Improve patient care systematically with InsiderCX
High-quality care is a continuous journey, not a one-time project. The most successful clinics iterate quickly: they listen to patients, empower staff, and measure relentlessly.
InsiderCX streamlines that cycle by:
- Capturing feedback from SMS/WhatsApp surveys, kiosks, and review sites in one dashboard.
- Surfacing real-time alerts on emerging hot spots (e.g., rising wait-time complaints).
- Linking staff actions — training completions, protocol adherence — to patient-experience trends.
- Auto-reporting quality metrics such as NPS and review scores for leadership and regulators.
Stat improving care quality with InsiderCX. Schedule a demo, start a pilot project, and get the data you need to deliver high-quality patient care.




