Healthcare is changing rapidly, and the patients of today are more informed, more selective, and expect the same level of personalised service they experience in other industries. This trend is driving the rising competition among private clinics and reshaping the way providers engage with patients.
At the heart of this shift is patient-centered care — an approach that prioritises the individual’s needs, preferences, and experience at every stage of their journey. To make that possible, clinics need more than clinical excellence; they need a systematic way to build, manage, and strengthen patient relationships.
That is the idea behind patient relationship management (PRM). Healthcare providers are increasingly recognising the value of PRM as a driver of trust, loyalty, and long-term growth.
Let’s see how it works and how to apply it on the clinic floor.
What is PRM in healthcare?
Patient relationship management refers to the strategies, processes, and technologies that clinics use to manage every interaction with their patients. Its purpose is to create a seamless, consistent experience, from the first enquiry and appointment scheduling to treatment and the subsequent follow-ups.
A useful way to understand PRM is to compare it with Customer Relationship Management (CRM) in other industries. The principles are similar — centralised data, personalised communication, measurable outcomes — but the end goal in healthcare is better health outcomes and increased patient retention.
For private clinics, improving PRM delivers palpable benefits:
- Stronger patient loyalty: Patients who feel valued and supported are more likely to return and recommend your clinic.
- Higher satisfaction scores: More engaged patients, combined with systematic management of the patient journey, result in consistently positive experiences.
- Operational efficiency: Streamlined communication and centralised data reduce bottlenecks and duplicated work.
- Better health outcomes: When patients are more engaged and informed, they are more likely to adhere to their treatment.
- Sustainable growth: Loyal patients and positive word-of-mouth directly support the clinic's reputation and growth.
The components of patient relationship management
An effective PRM strategy ensures that you’re putting the right structures in place to support consistent, patient-centered care. At its core, PRM brings together engagement, personalisation, technology, and workflow integration. Each of these elements plays a distinct role in building stronger relationships and better outcomes.
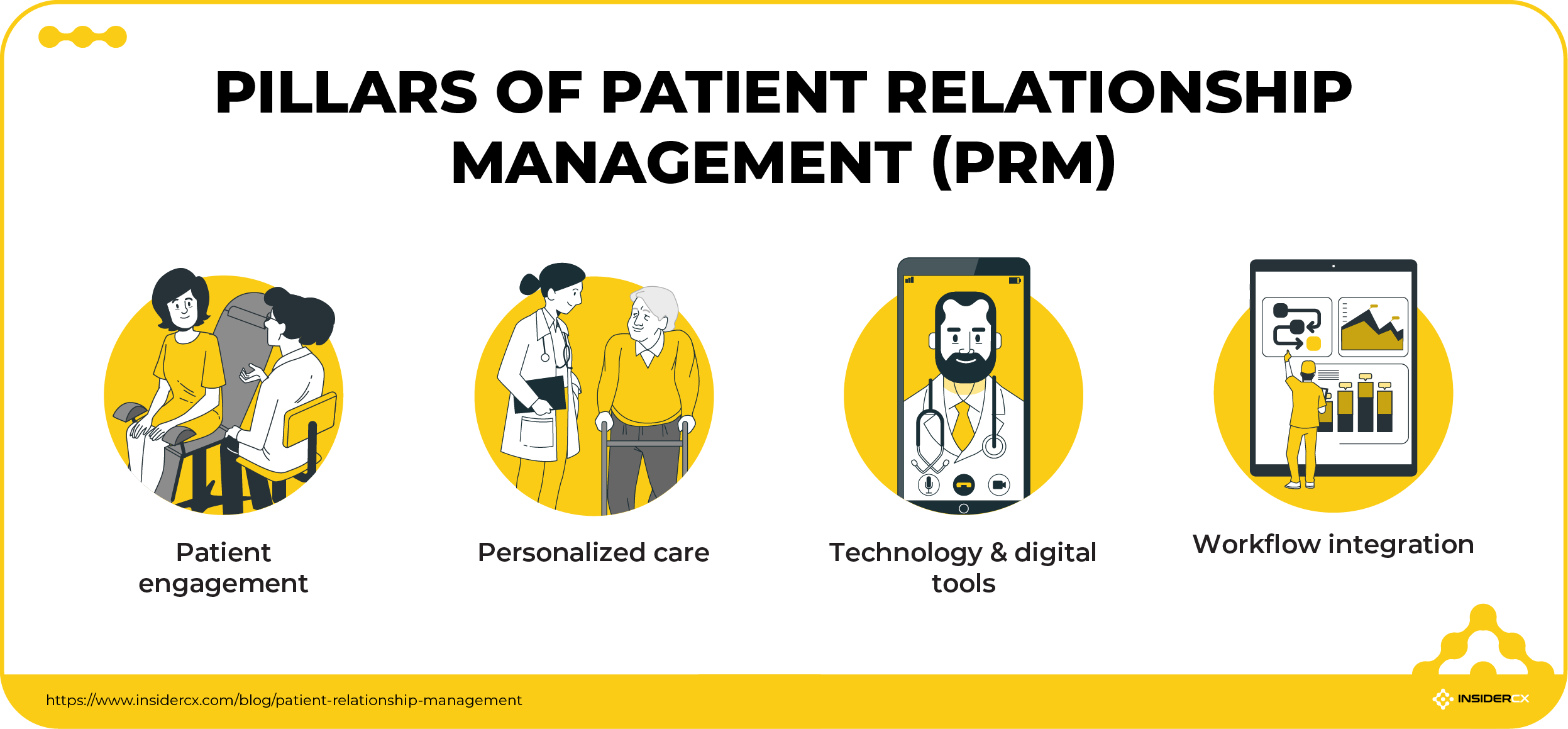
Patient engagement
Patient engagement is the foundation of PRM. It goes beyond providing information. Clinics should strive to establish a two-way dialogue where patients feel heard, informed, and actively involved in their own care.
When patients are active participants rather than passive recipients, their experience improves — and so do clinical outcomes. Engagement happens through clear communication, ongoing education, and shared decision-making, which builds trust and increases adherence to treatment plans.
You can use PAM surveys to measure how engaged and activated your patients are (and adjust care strategies accordingly).
Personalized care
No two patients are alike. To personalize the care they provide, clinics can make use of patient data to:
- Provide reminders for preventive screenings
- Adjust communication based on age and other demographic data
- Recognise patient preferences and expectations
- Create tailored treatment recommendations
- Proactively follow up on specific conditions
- Adjust care pathways based on lifestyle factors.
By meeting patients where they are, you demonstrate empathy and commitment. Both of which translate directly into loyalty and satisfaction.
Technology & digital tools
Modern PRM relies heavily on digitalization. Tools such as patient portals, mobile apps, telehealth, electronic health records (EHR), CRM systems, and automated reminders make it easier to deliver care that is accessible, efficient, and personalised.
Technology can reduce friction across the patient journey — from booking appointments and accessing test results to receiving medication reminders and joining virtual consultations. Plus, it also empowers clinics with data to monitor performance and identify opportunities for improvement.
Workflow integration
For PRM to succeed, it must be embedded into everyday operations. That means aligning providers, nurses, and administrative staff around shared processes and ensuring that technology supports — rather than complicates — their work.
Workflow integration creates a smoother interplay between departments and reduces bottlenecks that frustrate both staff and patients.
An example would be a system we’ve implemented for some of our clients, where every piece of negative feedback automatically generates a “patient care ticket” in the clinic’s CRM. The ticket is assigned to the appropriate team member — whether clinical, administrative, or support — with full visibility into the patient’s history and survey responses.
This ensures quick follow-up calls, issue resolution, and closure tracking. The result is a proactive loop where no concern goes unnoticed, and patients see tangible proof that their inputs and concerns lead to action.
Steps for building a new patient relationship management strategy
Adopting PRM is not something clinics can achieve overnight. If you want to avoid common pitfalls, ensure staff buy-in, and deliver measurable improvements to patient experience, we’ve mapped out a step-by-step process.
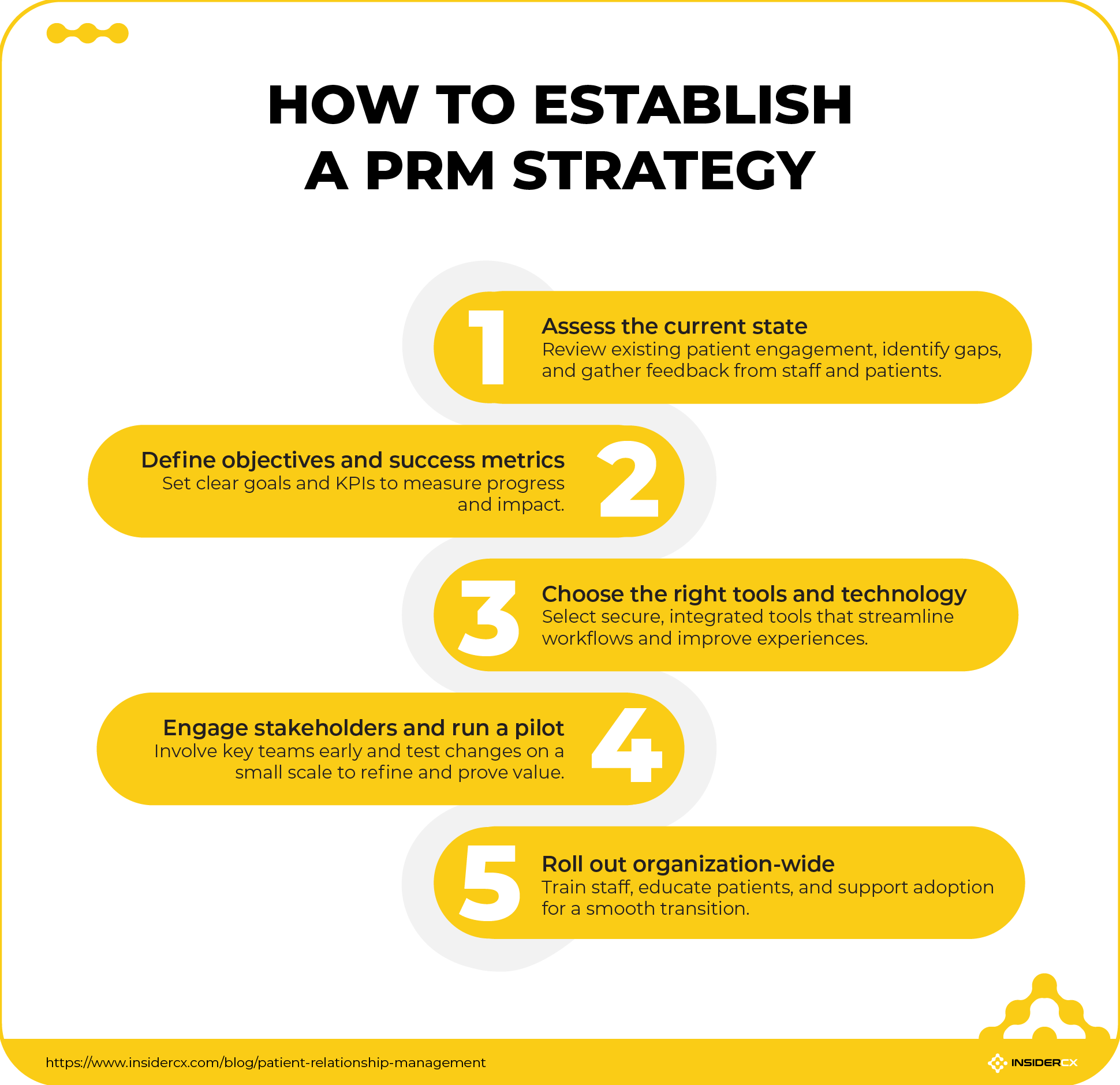
1. Assess the current state
The first step is to understand where you are today. Evaluate your existing patient engagement processes — how patients currently book appointments, receive information, and follow up after care.
Look for gaps in technology, workflows, and communication. Do patients struggle with reaching staff by phone? Are appointment reminders inconsistent? Does feedback get collected, but not acted upon?
Importantly, involve both patients and staff in this assessment. Patient and staff feedback reveals real-world pain points and ensures that improvements are grounded in actual needs.
2. Define objectives and success metrics
Once the baseline is clear, the next step is to decide where you want to go. Define clear, measurable objectives such as improving patient satisfaction, reducing no-shows, or increasing engagement with digital tools.
Then, establish the right KPIs to track progress, keep the strategy focused, and make it easier to demonstrate progress over time. You can look at metrics like:
- Patient portal adoption rates
- Net Promoter Score (NPS) or satisfaction scores
- Number of patient complaints
- Appointment adherence rates
- Average response time to patient enquiries
3. Choose the right tools and technology
Technology is the backbone of effective PRM, so choose tools that directly address the gaps you identified in step one. Prioritise solutions that can serve multiple functions. A modern patient experience platform should be able to consolidate these functions, making the system easier to manage and more effective for staff and patients alike.
Equally important, ensure that any chosen tools are compliant with GDPR, HIPAA, and other data security standards. They should also integrate seamlessly with your existing systems, such as EHRs, to avoid creating silos of information.
4. Engage stakeholders and run a pilot project
PRM initiatives succeed when everyone is involved from the start. Bring leadership, clinicians, administrative staff, and IT teams into the planning phase early. Similarly, before rolling out changes across the entire organisation, test them through a pilot project.
For example, at InsiderCX, we’ll usually roll out new features as pilots — and this is true for both our existing partners and for entirely new ones. This allows us to have a quick and efficient setup, a fast rollout, and be flexible with testing, tweaking, and defining features and workflows. It also enables us to gather and analyse data very quickly, showcase the benefit of a new feature or partnership, and it’s a great tool for identifying (and resolving) unforeseen issues on a smaller scale.
For new partners, we usually run a one-month proof-of-concept pilot which is essentially a trial run of our platform. It’s a limited number of messages sent, all crunched into a dashboard, and it’s our way of showing that changes can be seen and felt even on a limited run of patients surveyed.
5. Roll out the changes across the organization
With pilot results in hand, adjust workflows and processes as needed, then move to full-scale implementation. Provide training for your team so they feel confident using new tools and processes.
Equally important — educate your patients. Introduce them to new portals, messaging apps, or telehealth options and explain the benefits clearly: faster access, easier communication, and more personalised care.
Rolling out PRM successfully is as much about change management as it is about technology. The more supported and informed both staff and patients feel, the smoother the transition will be.
Challenges in implementing PRM
Big changes always come with a certain amount of friction. PRM is no exception. Healthcare organisations often face hurdles that need to be anticipated and addressed early. Some of the most common include:
- Data security and HIPAA compliance: Protecting sensitive patient data is non-negotiable. PRM systems must comply with strict data privacy regulations such as HIPAA in the US or GDPR in Europe.
- Integration with EHRs: PRM tools need to work seamlessly with established clinical systems to avoid creating data silos and extra work for staff.
- Training healthcare staff and overcoming resistance to change: New workflows and technologies require training; staff may initially resist, so clinics must emphasise the benefits for both patients and teams.
- Balancing automation with a human touch: While digital tools streamline communication, they should never replace empathy. Successful PRM strategies combine efficiency with personalised, human-centred care and communication.
Addressing these challenges head-on will create a smoother path to adoption.
Measure the success of your PRM strategy with InsiderCX
With InsiderCX, healthcare organisations can track patient feedback on a daily, weekly, and monthly basis, monitor satisfaction scores and online reviews, and identify the key drivers behind patient loyalty and engagement.
These insights make it possible to see whether PRM and other initiatives are truly working as intended.
InsiderCX helps clinics transform their PRM strategy into a continuous improvement cycle, and we do that by aligning patient feedback with organisational KPIs.
The results are stronger relationships, better outcomes, and a more patient-centred healthcare experience.




