Clinical audits have long been a cornerstone of healthcare quality. But in many organisations they still feel like a periodic obligation rather than an operational advantage.
Modern healthcare operates under constant pressure from all verticals. In this environment, clinics (especially those in the private sector) should leverage audits to improve service quality and satisfaction, not just verify compliance.
In this guide, you’ll learn what a clinical audit is, how it fits into broader quality improvement efforts, and the practical steps healthcare teams can follow to run audits efficiently and consistently.
What is a clinical audit?
A clinical audit is a structured process used to assess whether care is being delivered in line with the defined standards and practices.
The core purpose of clinical audits is to identify where care meets expectations, where it falls short, and what should change to improve patient outcomes and service quality. As such, they often act as the starting point for quality improvement (QI) initiatives.
Depending on the organisation's size, healthcare audits can be conducted by individual clinicians or multidisciplinary teams. In many cases, leadership or governance teams provide oversight, while frontline professionals contribute data and insights. Successful audits rely much more on collaboration than on ownership by a single role.
In the UK, clinical audits play a recognised role within healthcare governance frameworks. Initiatives such as the National Clinical Audit and Patient Outcomes Programme (NCAPOP), managed by the Healthcare Quality Improvement Partnership (HQIP), collect and analyse data from participating providers to provide a national picture of care standards for specific conditions.
How to do a clinical audit (by following the audit cycle)
To ensure repeatability and benchmarking, clinical audits should have a specific structure. While terminology may vary slightly between organisations, most follow a similar sequence. Let’s break it down.
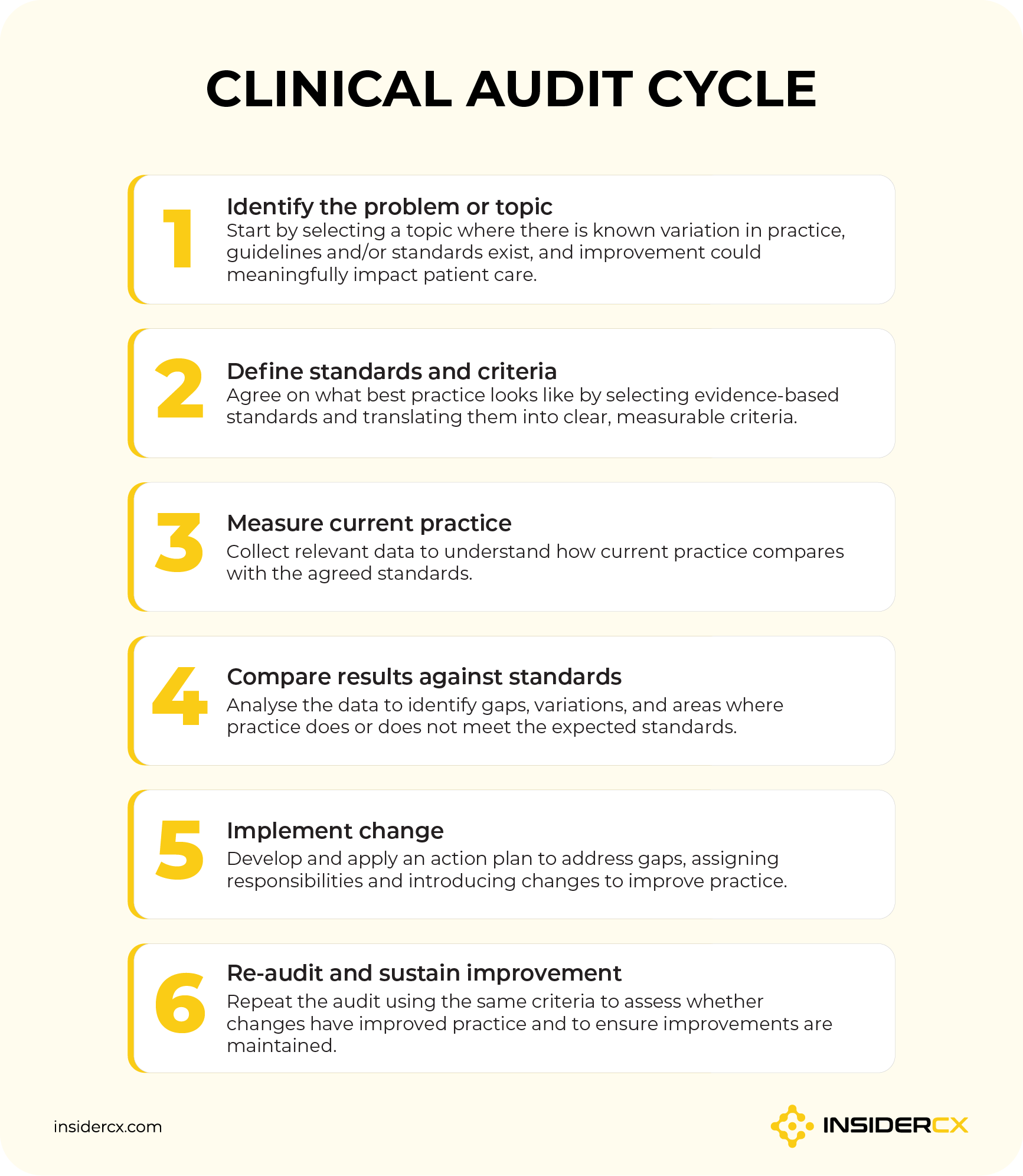
Step 1: Identify the audit topic
Choosing a topic helps define the scope of the audit. The most effective healthcare audits focus on areas where improvement can meaningfully impact patient outcomes, safety, or service quality.
Strong candidates often share common characteristics:
- There is known variation in practice or outcomes.
- Clear guidelines or standards already exist.
- Improvement would significantly benefit patients or reduce operational risk.
Audit topics should also align with national guidelines, organisational policies, or known performance gaps. Involving stakeholders (clinicians, operational leads, and sometimes even patients) helps ensure the audit addresses real-world priorities rather than theoretical concerns.
Step 2: Define standards and criteria
Once a topic is selected, the next step is defining what “good” looks like. Standards typically come from national clinical guidance, regulatory expectations, or evidence-based best practice.
However, standards alone are not enough; they must be translated into measurable criteria.
In simple terms, a standard describes the desired level of performance; criteria define how performance will be measured against that standard. For example, a guideline may state that discharge instructions must be clearly communicated. The audit criteria might specify measurable indicators such as documented patient understanding or provision of written follow-up information.
Setting realistic performance targets is equally important. Targets should be ambitious enough to drive improvement but achievable within operational constraints.
Step 3: Plan the audit
A well-defined plan prevents audits from becoming overly complex or resource-heavy.
Key planning considerations include:
- Defining the audit’s scope and objectives clearly.
- Identifying relevant data sources, such as electronic health records, patient feedback, or operational reports.
- Determining sample size and timeframe to ensure findings are meaningful without becoming burdensome.
- Reviewing ethical considerations and approvals if required, particularly when patient-identifiable data is involved.
Clear planning ensures consistency and makes the audit easier to repeat later when measuring improvement.
Step 4: Collect the required data
Clinical audits can combine both quantitative and qualitative data.

Quantitative data may include compliance rates, timeframes, satisfaction metrics, or clinical outcome measures, while qualitative insights — such as open-text patient feedback, interviews, or clinician observations — provide context that numbers alone cannot capture.
Common data collection methods include chart reviews, structured surveys, electronic health record extraction, and direct observation. Regardless of the method, maintaining data accuracy, confidentiality, and consistency is essential to ensure credible results.
Step 5: Analyse and benchmark collected data
Once data is collected, the goal is to compare current practice against predefined standards.
This involves identifying gaps, variations between teams or locations, and potential root causes. Wherever possible, compliance should be quantified, e.g. through percentages, rates, or benchmark comparisons.
And let’s not forget: clear presentation matters as much as analysis itself. Tables, charts, and dashboards help teams understand findings quickly and support meaningful discussions about improvement priorities.
Step 6: Discuss and implement changes
Audit findings should, above all, lead to action. This stage involves reviewing results collaboratively with relevant teams and identifying practical improvements.
Common interventions include training or coaching initiatives, updates to clinical protocols and workflows, all the way to changes in systems, documentation, or communication processes.
Action plans should define responsibilities, timelines, and success measures. Without clear ownership, you’re running the risk of well-designed audits becoming passive reports — and not the drivers of change you set out to establish.
Step 7: Re-audit for ongoing improvement
The audit cycle is only complete once organisations return to measure progress. Re-auditing closes the loop by transforming clinical audits from static assessments into continuous improvement mechanisms.
After allowing sufficient time for changes to take effect, teams should repeat data collection using the same criteria. This makes it possible to assess the improvements and determine whether standards are now being met.
An example of a clinical audit
Recently, one of our clients, Poliklilnika Aviva, used patient feedback as part of its quality management framework while preparing for dual accreditation under AACI and ISO 7101 standards.
Rather than treating accreditation as a one-time inspection exercise, leadership defined targeted audit topics focused on communication quality, consistency, and service delivery standards — all in line with the requirements from the auditors.
To align with accreditation requirements, Aviva translated quality expectations into measurable criteria, using structured patient feedback to evaluate performance against defined standards. An automated patient feedback system enabled the organisation to gather consistent insights at scale, helping teams identify variations in care delivery, benchmark performance, and prioritise improvements.
Based on audit findings, Aviva implemented workflow improvements and strengthened internal communication processes. This continuous feedback loop provided measurable proof of quality performance during ISO and AACI assessments.
This is a perfect example of how healthcare audits can move beyond mere compliance and become a practical driver of sustained organisational improvement.
Tools to help streamline the audit process
Clinical audits can be time-consuming and difficult to sustain if they rely entirely on manual tracking or ad-hoc processes. The right tools reduce administrative burden, improve consistency, and make it easier to repeat the audit cycle over time.
Audit software
This is software designed to support the structured audit cycle by centralising planning, data collection, analysis, and reporting in one place. Instead of managing multiple documents and disconnected data sources, teams can follow through the entire audit and generate reports within a single system.
Typical capabilities include:
- Structured audit templates
- Automated scoring against defined criteria
- Progress tracking
- Visual dashboards that highlight compliance levels and trends.
Examples: Radar Healthcare, Audit Angel, and other general audit software.
Clinical audit survey
A clinical audit survey is a structured questionnaire used to collect targeted data related to specific audit criteria. Unlike general patient satisfaction surveys, audit surveys focus on measurable indicators linked to defined standards.
These surveys can be completed by clinicians, patients, or administrative staff, depending on the area being audited. When automated through digital platforms, they allow organisations to gather large volumes of consistent data quickly.
For example, a clinic auditing communication quality might use post-visit surveys to evaluate whether patients felt informed about next steps, providing real-time insight into adherence to communication standards.
Patient experience survey platforms like InsiderCX help streamline this process by automatically collecting structured patient feedback and converting it into actionable quality metrics.
Templates and checklists
Templates and checklists provide a simple but highly effective way to standardise clinical audits — especially for teams starting to formalise their QA processes.
Common examples include:
- Clinical documentation review checklists.
- Patient journey mapping templates.
- Procedure or pathway compliance templates.
- Communication quality scoring sheets.
- Audit planning templates outlining objectives, criteria, and timelines.
These tools help apply the same criteria consistently, maximally reducing subjectivity.
Over time, reusable templates also help organisations build institutional memory, allowing future audits to start from proven frameworks rather than reinventing the process each time.
Best practices for successful clinical audits
While the audit cycle provides structure, success ultimately depends on how well you can execute each of the phases. Let’s take a closer look at some of the key best practices.
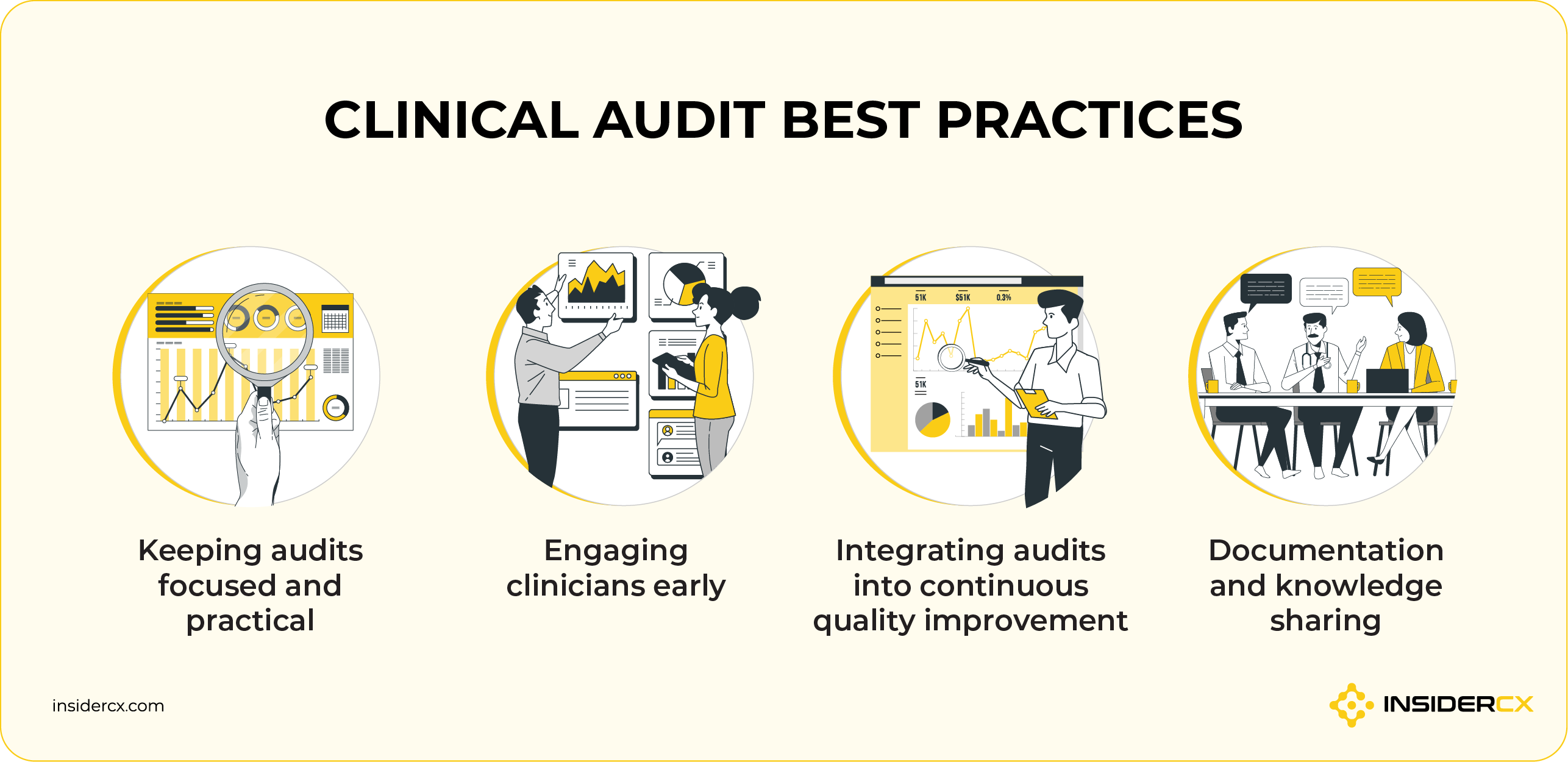
Keeping audits focused and practical
One of the most common pitfalls is trying to audit too much, all at once. Successful audits narrow the scope to manageable objectives that teams can realistically measure and act upon.
Focusing on areas with clear potential for improvement — instead of collecting excessive or overly complex data — helps maintain momentum and prevents audits from becoming administrative burdens. Remember, the goal is actionable insight, not hoarding data.
Engaging clinicians early
Involving clinicians during topic selection and planning increases relevance and ownership. Clearly communicating the purpose of the audit, as well as its potential benefits for patient care and workflow improvement, reduces scepticism.
Encouraging multidisciplinary participation also ensures that operational, clinical, and patient experience perspectives are reflected in both analysis and implementation.
Integrating audits into continuous quality improvement
Clinical audits are most effective when they feed directly into ongoing quality improvement initiatives rather than being standalone exercises.
Audit findings should be the source of truth for policy updates, targeted training, staff development initiatives, and process redesign. When audits are a part of a continuous improvement cycle, teams begin to see them as tools for learning and refinement rather than simple evaluation activities.
Documentation and knowledge sharing
Clear documentation ensures that audit insights don’t get lost over time. Recording methods, criteria, results, and actions creates a reusable knowledge base that supports future re-audits.
Sharing findings across teams and departments accelerates organisational learning, helping best practices take root and preventing avoidable mistakes. Strong documentation also supports governance requirements and provides evidence of continuous improvement efforts when needed.
Don’t sleep on data quality!
At their core, audits exist to improve patient outcomes by identifying gaps between current practice and predefined standards — but inaccurate, incomplete, or biased data can lead teams toward the wrong conclusions.
Without high-quality data, audits can become mere compliance exercises.
This is where modern, healthcare-focused tools like InsiderCX play an increasingly important role. They help clinics collect structured patient feedback at scale, translating real-world patient experiences into measurable insights.
Once you’re able to automate data collection and ensure consistency across locations, you’re essentially getting a larger, more representative sample size — allowing your organization to move beyond anecdotal feedback and make decisions based on reliable evidence.
Clinical audit FAQs
What are examples of common clinical audit topics?
Clinical audits typically focus on areas where standards exist and measurable improvement is possible. Common examples include infection control compliance, medication safety processes, documentation quality, patient consent and communication practices, and adherence to screening or preventive care protocols.
How often should care providers conduct clinical audits?
There is no universal schedule. High-priority or high-risk areas may be audited continuously or annually, while targeted audits may occur as needed (when new risks, policy changes, or performance gaps emerge).
Are clinical audits performed internally or by external experts?
Most audits are conducted internally by clinical teams or quality governance staff because they understand local workflows and context. External experts may be involved for benchmarking, specialist audits, or independent validation.
What are the most common challenges with healthcare audits?
Even well-designed clinical audits encounter recurring operational and cultural obstacles that prevent them from translating findings into meaningful change. These include:
- Lack of data or poor data quality (incomplete, inconsistent, or poorly structured data that is hard to analyse).
- Busy clinical environments often struggle to dedicate sufficient staff time to structured auditing.
- Low clinician engagement or unclear purpose when audits are perceived as a tedious compliance exercise.
- Without clear ownership or leadership support, audit findings remain theoretical rather than driving impactful change.
How does the InsiderCX platform improve healthcare audits?
InsiderCX strengthens clinical audits by automating the collection of structured patient feedback. Once the platform begins providing relevant and consistent data samples, it becomes easy to convert qualitative insights into measurable metrics that support benchmarking, analysis, and re-auditing.
In a nutshell, InsiderCX helps teams move from manual data gathering to continuous, evidence-driven improvement.